Clinical Correlates of Patients Who Had Pacemaker Implantation in Port Harcourt, Southern Nigeria
Main Article Content
Abstract
Background: Permanent pacemaker implantation is a relatively safe procedure that significantly improves morbidity and mortality among patients with symptomatic bradycardia. There is limited information on the clinical correlates of pacemaker patients in the south-south Nigeria, especially in a private tertiary cardiac clinic. This study is aimed at describing the clinical correlates as seen in patients who had pacemaker implantation in a private hospital in Port Harcourt, Southern Nigeria.
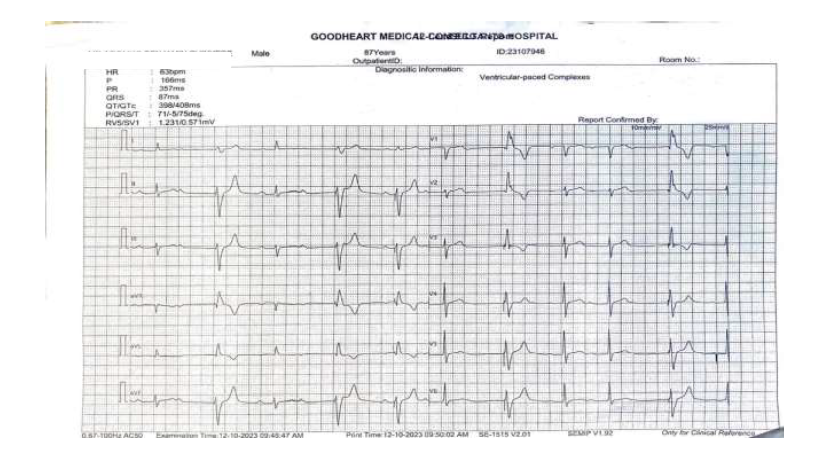
Materials and Methods: This was a retrospective study of patients who had pacemaker implantation in the University of Port Harcourt Teaching hospital from 2012 to 2013 and GoodHeart Medical Consultants Hospital in Port Harcourt, Southern Nigeria from 2014 to 2023.
Results: The mean age (±SD) of total population at the time of implantation was 66.8 (±10.6) years. Men were more than the women (51.8% vs. 48.2%). Single-chamber unit was mostly implanted, single-chambers were in 25 (60.98%) while Dual chamber units were implanted in 16 (39.02%) of patients. Complete heart block (CHB) was the most common (60.98%) indication for permanent pacemaker insertion followed by second degree atrioventricular block (29.27%) and other indications (9.76%). The most common presenting symptoms were dizziness (in 56.1% of patients), blackout (24.4%), and dyspnea (19.5%). The complications observed were Lead dislodgment/malfunction, pocket infection in 3 patients each, and device expulsion in 2 patients.
Conclusion: Pacemaker implantation in Port Harcourt south-south, Nigeria started in September 2012. There was great apathy and inertia on the side of patients and their relations as well as poor infrastructures, hence, the few numbers of patients at the onset. The major reason for pacemaker implantation were complete heart block (CHB) and second degree Atrioventicular block (2nd degree AVB). Pacemaker implantation is a highly effective procedure in treatment of symptomatic bradycardia. It is a lifesaving procedure as it improves quality of life and is associated with relatively low complications and has now achieved a wider acceptance among the populace.
Article Details
References
Kanse VY, Chongtham DS, Salam KS, Nemichandra SC, Upretti S, Singh SD. Clinical profiles and outcomes of patients undergoing pacemaker implantation. J Med Soc. 2015 Apr;29(1):40.
Lopez-Jimenez F, Goldman L, Orav EJ, Ellenbogen K, Stambler B, Marinchak R, et al. Health values before and after pacemaker implantation. Am Heart J. 2002 Oct 1;144(4):687–92.
Khanal J, Poudyal RR, Devkota S, Thapa S, Dhungana RR. Clinical Profile and Early Complications after Single and Dual Chamber Permanent Pacemaker Implantation at Manmohan Cardiothoracic Vascular and Transplant Centre, Kathmandu, Nepal. 2015 [cited 2024 Feb 28]; Available from: http://elibrary.nhrc.gov.np:8080/handle/20.500.14356/1750
Thomas MO. Acceptance of Elective Bradypacing by Patients: An African Perspective. Pacing Clin Electrophysiol. 2012;35(1):58–61.
Nwafor CE. Cardiac pacemaker insertion in the South-South Region of Nigeria: Prospects and challenges. Niger Health J. 2015;15(3):125–30.
Kotsakou M, Kioumis I, Lazaridis G, Pitsiou G, Lampaki S, Papaiwannou A, et al. Pacemaker insertion. Ann Transl Med. 2015 Mar;3(3):42.
Ahmed M. Patients characteristic, indications, and complications of permanent pacemaker implantation: A prospective single-center study. Med J Babylon. 2022;19(2):152.
Eltrafi A, Currie P, Silas JH. Permanent pacemaker insertion in a district general hospital: indications, patient characteristics, and complications. Postgrad Med J. 2000 Jun 1;76(896):337–9.
Shenthar J, Bohra S, Jetley V, Vora A, Lokhandwala Y, Nabar A, et al. A survey of cardiac implantable electronic device implantation in India: By Indian Society of Electrocardiology and Indian Heart Rhythm Society. Indian Heart J. 2016 Jan 1;68(1):68–71.
Authors/Task Force Members, Brignole M, Auricchio A, Baron-Esquivias G, Bordachar P, Boriani G, et al. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: The Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur Heart J. 2013 Aug 1;34(29):2281–329.
Harcombe AA, Newell SA, Ludman PF, Wistow TE, Sharples LD, Schofield PM, et al. Late complications following permanent pacemaker implantation or elective unit replacement. Heart. 1998 Sep 1;80(3):240–4.
Edafe EA, Odia JO, Akpa MR, Dodiyi-Manual ST, Oye H, Agadah Z. Experience with cardiac pacing in the Nigerian Delta region. Niger J Cardiol. 2020 Dec;17(2):136.
Ellenbogen KA, Hellkamp AS, Wilkoff BL, Camunãs JL, Love JC, Hadjis TA, et al. Complications arising after implantation of DDD pacemakers: the MOST experience. Am J Cardiol. 2003 Sep 15;92(6):740–1.
Edwards SJ, Karner C, Trevor N, Wakefield V, Salih F. Dual-chamber pacemakers for treating symptomatic bradycardia due to sick sinus syndrome without atrioventricular block: a systematic review and economic evaluation. Health Technol Assess. 2015 Aug 24;19(65):1–210.
Permanent pacemaker implantation after open heart surgery - Turkish Journal of Thoracic and Cardiovascular Surgery [Internet]. [cited 2024 Mar 6]. Available from: https://tgkdc.dergisi.org/abstract.php?lang=tr&id=970
Onakpoya UU, Ojo OO, Eyekpegha OJ, Oguns AE, Akintomide AO. Early experience with permanent pacemaker implantation at a tertiary hospital in Nigeria. Pan Afr Med J [Internet]. 2020 Jul 13 [cited 2024 Feb 28];36(1). Available from: https://www.ajol.info/index.php/pamj/article/view/213237
Ekpe EE, Aghaji MA, Edaigbini SA, Onwuta CN, Anisiuba B. Cardiac pacemaker treatement of heart block in Enugu: a 5 year review. Niger J Med. 2008 Apr 22;17(1):7–12.
Aktoz M, Uçar MF, Yılmaztepe MA, Taylan G, Altay S. Gender Differences and Demographics and Type of Cardiac Device over a 10-Year Period. Niger J Clin Pract. 2018;21(1):27–32.
Falase B, Sanusi M, Johnson A. Analysis of a five year experience of permanent pacemaker implantation at a Nigerian Teaching Hospital: Need for a national database. Pan Afr Med J [Internet]. 2014 May 5 [cited 2024 Mar 7];16(1). Available from: https://www.ajol.info/index.php/pamj/article/view/103275
Adeoye PO, Okonta KE, Salami MA, Adegboye VO. Experience with permanent pacemaker insertion at the University College Hospital, Ibadan, Nigeria. Niger J Cardiol. 2013 Jun;10(1):3.
Alpert MA, Curtis JJ, Sanfelippo JF, Flaker GC, Walls JT, Mukerji V, et al. Comparative survival after permanent ventricular and dual chamber pacing for patients with chronic high degree atrioventricular block with and without preexistent congestive heart failure. J Am Coll Cardiol. 1986 Apr 1;7(4):925–32.
Trohman RG, Kim MH, Pinski SL. Cardiac pacing: the state of the art. The Lancet. 2004 Nov;364(9446):1701–19.
Res JCJ, de Priester JA, van Lier AA, van Engelen CLJM, Bronzwaer PNA, Tan PH, et al. Pneumothorax resulting from subclavian puncture: a complication of permanent pacemaker lead implantation. Neth Heart J. 2004 Mar;12(3):101–5.
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR, Committee THICPA. Guideline for Prevention of Surgical Site Infection, 1999. Infect Control Hosp Epidemiol. 1999 Apr;20(4):247–80.
Bonny A, Ngantcha M, Jeilan M, Okello E, Kaviraj B, Talle MA, et al. Statistics on the use of cardiac electronic devices and interventional electrophysiological procedures in Africa from 2011 to 2016: report of the Pan African Society of Cardiology (PASCAR) Cardiac Arrhythmias and Pacing Task Forces. EP Eur. 2018 Sep 1;20(9):1513–26.